Pneumonia is a common respiratory infection characterized by inflammation of the air sacs in one or both lungs. It can be caused by various pathogens, including bacteria, viruses, and fungi, and can range from mild to severe, potentially leading to complications, especially in vulnerable populations. Understanding the causes, symptoms, diagnosis, and treatment of pneumonia is essential for timely intervention and optimal management. In this blog post, we unravel the intricacies of pneumonia to empower readers with valuable insights into this prevalent respiratory condition.
Causes of Pneumonia:
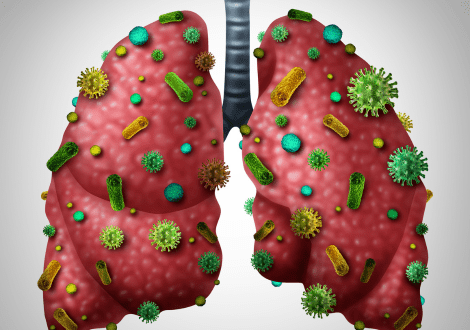
Pneumonia can be caused by a wide range of microorganisms, with the most common culprits being bacteria and viruses. Some of the primary causes of pneumonia include:
- Bacterial pneumonia: Bacteria such as Streptococcus pneumoniae, Haemophilus influenzae, and Mycoplasma pneumoniae are common causes of bacterial pneumonia, particularly in adults.
- Viral pneumonia: Viruses, including influenza (flu), respiratory syncytial virus (RSV), and adenovirus, can infect the lungs and lead to viral pneumonia, often affecting young children and older adults.
- Fungal pneumonia: Fungi such as Pneumocystis jirovecii (common in individuals with weakened immune systems) and Histoplasma capsulatum (common in certain geographic regions) can cause fungal pneumonia.
- Aspiration pneumonia: Inhalation of food, drink, saliva, or vomit into the lungs can lead to aspiration pneumonia, especially in individuals with swallowing difficulties or impaired consciousness.
Symptoms of Pneumonia:
The symptoms of pneumonia can vary depending on the cause, severity, and individual factors. Common symptoms include:
- Cough, which may produce phlegm (sputum) that can be clear, yellow, green, or bloody
- Fever, with or without chills
- Shortness of breath or difficulty breathing
- Chest pain that worsens with breathing or coughing
- Fatigue and weakness
- Rapid heartbeat
- Bluish discoloration of the lips or nails (cyanosis) in severe cases
Diagnosis of Pneumonia:
Diagnosing pneumonia typically involves a combination of medical history evaluation, physical examination, and diagnostic tests. Common diagnostic tests for pneumonia include:
- Chest X-ray: Imaging studies such as chest X-rays can reveal abnormalities in the lungs, including areas of inflammation and consolidation characteristic of pneumonia.
- Blood tests: Blood tests, including a complete blood count (CBC) and blood cultures, can help identify signs of infection and determine the causative organism.
- Sputum culture: Analyzing a sample of sputum coughed up from the lungs can help identify the specific pathogen causing pneumonia, particularly in cases of bacterial or fungal pneumonia.
- Pulse oximetry: This non-invasive test measures the oxygen saturation of the blood and helps assess the severity of pneumonia and the need for oxygen therapy.
Treatment of Pneumonia:
Treatment of pneumonia depends on the underlying cause, severity of symptoms, and individual factors. Common treatment approaches include:
- Antibiotics: Bacterial pneumonia is typically treated with antibiotics, with the choice of antibiotic guided by factors such as the suspected pathogen, local resistance patterns, and the patient’s clinical condition.
- Antiviral medications: Viral pneumonia caused by influenza or other respiratory viruses may be treated with antiviral medications, although supportive care is often the mainstay of treatment.
- Antifungal medications: Fungal pneumonia requires treatment with antifungal medications tailored to the specific fungal species identified through diagnostic testing.
- Supportive care: Supportive measures such as rest, adequate hydration, and over-the-counter pain relievers can help alleviate symptoms and promote recovery.
- Hospitalization: Severe cases of pneumonia, especially those associated with complications or compromised respiratory function, may require hospitalization for close monitoring and intravenous antibiotics or supportive therapies.